The case is increasingly made, that the structures and processes involved in knowledge production, use, and circulation in global health have epistemic injustice written all over them. But how are these justice concerns related to global health governance? Where does epistemic injustice meet global health governance?
Let us define epistemic injustice. Epistemic injustice occurs when the knowledge held by people who belong to marginalised groups (or their status as knowers or producers and recipients of knowledge) is systematically afforded less credibility; and when their interpretive or sensemaking resources (i.e. how they make sense of their experiences and of the world and their place in it) are not recognised.
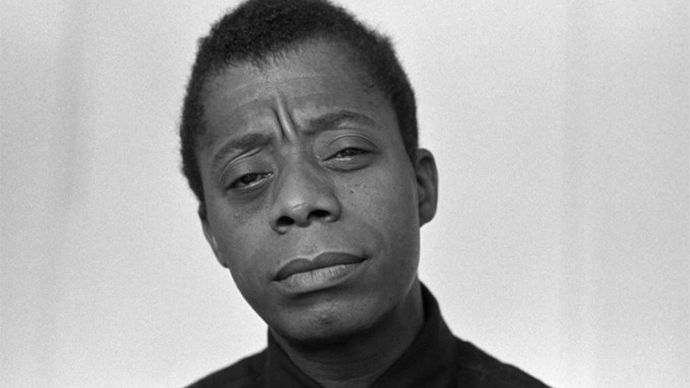
We do global health from a position of relative power. Our work involves working at a distance; or across divides of power, income, culture, ethnicity, race, class, status, et cetera. Across divides, we can only grasp a tiny slice of the complex social systems and realities that we seek to alter. Power and ignorance are in lockstep, with consequences for addressing health issues. As James Baldwin once wrote, “ignorance, allied with power, is the most ferocious enemy justice can have.”
Global health governance is much less easy to define. It is the kind of concept that means different things to different people. But I really like how Kelley Lee and Adam Kamradt-Scott reviewed the literature and identified three meanings of ‘global health governance’ – first, as globalisation and health governance (i.e. the institutional actors, arrangements and policy making processes that govern health issues in a globalised world); second, as global governance and health (i.e. how global governance institutions outside of the health sector influence the social, political, or commercial determinants of health), and third, governance for global health (i.e., normatively, about governance arrangements needed to achieve goals such as global health equity and access to medicines).
First, epistemic injustice meets global health governance in how globalisation intersects with health governance. Epistemic injustices occur because of the colonial imprints of globalisation. Knowledge systems are centralised (and by default, Western) and biased towards what a dominant, distant or foreign group values, how it makes sense of the world, and what it seeks to achieve. Avoiding and undoing epistemic injustices require deliberate action by the institutional actors that govern health issues in a globalised world – the World Health Organisation, and the institutional actors that set, monitor and enforce the norms that govern the knowledge ecosystem in global health – academic journals (and their publishers), research and training institutions, funding agencies, et cetera.
Second, epistemic injustice meets global health governance in how global governance affects health; how the governance of non-health global institutions affects health. You may think of the academic publishing industry (a non-health global institution) as a commercial determinant of health – if you consider how the industry gatekeeps the emergence of local journals (that can serve local needs and help connect local actors to local knowledge and build local knowledge ecosystems) out of academic publishing – by strategically raising the costs of entry and branding them as predators. Or you may consider how the global institution of academia biases researchers within and outside the academy from primarily serving the knowledge needs of the local settings where they work.
Third, epistemic injustice meets global health governance in its normative framing in terms of the governance arrangements necessary to achieve global health goals. Establishing normative frameworks to ensure that knowledge production, use, and circulation are optimised to achieve global health goals should a responsibility of institutional actors that govern global health.
Much too often, falsehoods are perpetuated and wrong interventions are promoted because local experts are excluded from owning the production and interpretation of knowledge that determines their destiny; or because knowledge produced by them is not deemed legitimate; or because they’re not recognised as audience of knowledge that is produced in their setting, or don’t see themselves as audience of such knowledge because of where or how it is published, whose knowledge gap it addresses or whose interpretations it reflects. Instances of epistemic injustice like these won’t undo themselves. They require deliberate action by or against actors involved in global governance.
Epistemic injustice should be spoken of more in the context of ‘global health governance’. We must draw attention to instances of epistemic injustice in how global health governance operates; and to how the institutions of global governance may be deployed to address epistemic injustices. This may sound trivial in a world grappling with pandemics and a climate crisis. But efforts to address these global (health) issues are more likely to fail if we don’t put in place governance structures and processes to ensure that every person (and group) is treated equally in their capacity as a knower.





